The interest in mass screening people for fever has launched a renewed interest in non-invasive thermometry and the use of infrared devices for such applications. In the past we have seen that choosing the right thermometer for a mass screening is vital. Otherwise a mass screening will do little to detect actual fevers. Even worse, it will give governments, health authorities, employers and individuals a false sense of security that carriers of COVID-19 are being successfully detected.

The temporal artery
The temporal artery area is a site with a long history of temperature measurement dating back centuries. The temporal artery is easily accessible because it lies 1 or 2 mm below the skin on the forehead. Also there are no mucous membranes present, thereby eliminating the risk of contaminates.
The temperature at the outer surface of the head is not the same as the arterial temperature of interest, since there is local cooling of the arterial blood supply due to a variety of local influences at the skin.
The frontal branch of the superficial temporal artery demonstrates the necessary requirements for the skin thermometry method:
- it is easily accessible
- contains no mucous membranes
- despite lying so close to the skin surface, it presents no risk of injury from being touched
- and most importantly, it has no or very few arteriovenous anastomoses (AVA)
Lack of AVA’s means that the perfusion rate is reliable under essentially all conditions, and the blood flow is relatively free of vasomotor control in response to thermomoregulatory stimuli. The high and reliable perfusion allows accurate mathematical computations of the heat lost to the environment due to the cutaneous flow. That is very important because it allows for an accurate calculation of the source arterial temperature at the heart.
Artery Heat Balance and Heat Loss Coefficient
The method of correcting the temperature for the cooling effect at the skin is called Artery Heat Balance or AHB. The AHB equation provides a measure of the heat transferred to the tissue by arterial blood and the heat loss at the skin to the ambient environment.
The AHB equation is completely general for so called steady state conditions. But here we run into a difficult to solve problem: when doing a mass screening (or any measurement that is) we do not have these ideal and steady state conditions. Especially when performing many measurements in a very short time. When evaluating the best thermometry for a mass screening it is important to look very carefully at the factors that impact the Artery Heat Balance of the researched thermometers.
Comparison of telemetry methods
So how does this apply to several thermometry methods?
- Ear thermometers – The heat loss coefficient is highly variable and depends very much on the direction the sensor is pointed when to sensor head or probe is inserted into the ear. Deep tissue near the tympanic membrane is well insulated. So it produces a low value of the heat loss coefficient and an accurate temperature. On the other hand, superficial ear tissue is much more exposed. Because of that the ear thermometer will produce a completely different heat transfer coefficient that might be an order of magnitude greater than a measurement performed in the vicinity of the tympanic membrane. The perfusion rate is very low in the ear tissue. That means that it amplifies the variations in the heat loss coefficient. When a health worker is performing many measurements the result will be a highly variable measurement which produces differences of more than 1 oC depending on where the infrared sensor is pointed.
- Oral thermometry – Temperature measurements in the mouth are heavily influenced by evaporation, which dramatically influences the heat transfer coefficient. The impact depends on air motion in the oral cavity, the local dew point (did the individual recently drank coffee or tea or a glass of cold water?) and where exactly the thermometer is placed. The perfusion rate is very high in the oral cavity, which reduces the inaccuracy. Almost always the oral measurements result in a lower temperature than the arterial temperature. And depending on the factors mentioned above the measured temperature can vary significantly (± 1 oC).
- Rectal thermometry – Here the heat transfer coefficient is determined by the depth of insertion. This means the heat transfer coefficient can be variable, especially in infants. So that may lead to variable results. In most cases the perfusion rate is very low. There is an additional factor in play here though: low perfusion of a large tissue mass. When measuring the temperature of adults this can lead to an added lag time error of several hours. In other words: it may take a substantial amount of time before an elevated temperature or fever in the heart can be detected when using a rectal thermometer. Although rectal measurement usually are considered ‘the golden standard’ the factors mentioned above result in a measurement that is much more variable than is commonly assumed.
- Temporal Artery Thermometry – Temporal Artery Thermometers are very easy to use. That means that even in a mass screening the temporal artery on the forehead of an individual can be found without any difficulty. The heat loss coefficient has only small variations and depends on the local skin properties (except perspiration). This results in a very consistent measurement that is largely independent of the technique used by the health worker. By technique we mean the handling of the thermometer by the health worker. To neutralize the impact of perspiration the scan on the forehead may be extended to a spot on the neck behind the earlobe. This area remains relatively dry, even when other areas of the skin are wet from perspiration. That means the peak temperature will be measured even when the temporal artery is cooled by perspiration. The skin areas on the forehead and behind the earlobe have a perfusion rate that is close to that observed at the temporal artery. That means that a Temporal Artery Thermometer will produce an accurate body temperature by using the AHB equation calibrated for the temporal artery.
Temporal Artery Themometry versus IR guns (or any remote IR radiometer)
During the Corona virus outbreak we have seen the use of IR cameras and remote IR radiometers. Although these tools are non-invasive they are NOT suitable for a mass screening. The reason is that an IR camera or radiometer must contend with two sources of measurement uncertainty:
- the radiometer uncertainty
- the physiological uncertainty
It appears from specifications of the best devices that absolute accuracies for IR imagers are limited to about ±1 °C. Spot radiometers designed for medical applications can achieve absolute accuracies of 0,2 °C. The best (professional Temporal Artery Thermometers) achieve 0,1 °C absolute accuracy.
The large uncertainty for the remote IR device is consistent with observed poor performance in detecting fevers. Since the entire range of normal temperatures is only about 2 °C a measuring device with an sensitivity of 2 °C will have very poor sensitivity in fever detection. That will often lead to a very high number of false positives if adjustments are made to the fever threshold to improve sensitivity.
There may be some attractiveness to developing imagers with the physiological model improvements employed in Temporal Artery Thermometry for certain applications. However, it is very difficult to justify such an approach at airports, where each X-ray security point could be equipped with a highly competent and proven Temporal Artery Thermometer costing about $400, or even a light duty consumer model available in retail stores for $50, compared to an IR camera costing $50,000 to $100,000 which may not reliably detect fevers.
Our extensive experience with mass screening
With the outbreak of SARS in China there were extensive searches for thermometers which could be used for rapid non-invasive screening for fever. The Temporal Artery Thermometer was in heavy demand due to its proven clinical accuracy in fever detection. A number of factories in the affected areas used Temporal Artery Thermometry to scan workers prior to entering the factory, as well as schools, hospitals, businesses and places of worship.
One person with a Temporal Artery Thermometer can screen up to 600 persons per hour. This is a practical rate for a factory or an office. It can easily be used at airports which employ security procedures similar to those in the US, without any additional delay to the passenger.
Procedure for mass screening
This is the procedure we have developed based one our extensive experience during the SARS outbreak in China.
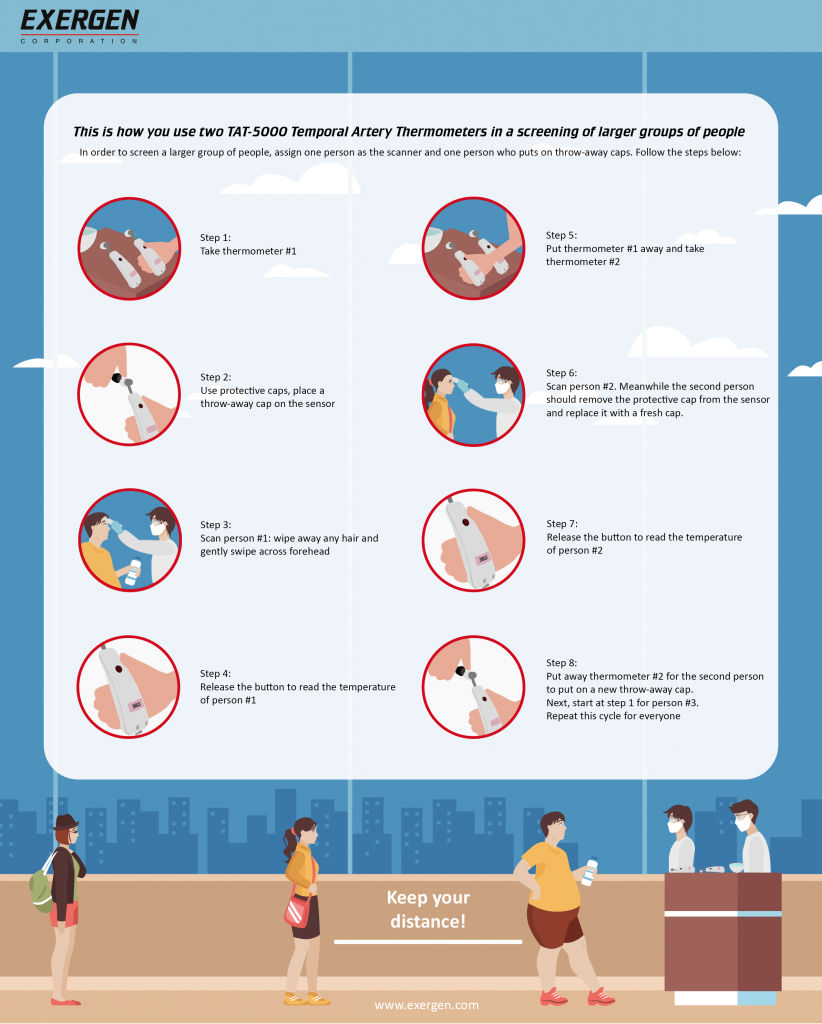
In order to scan a larger group of people assign two individual to the scanning process:
- scanner #1 is the individual who performs the actual measurements
- scanner #2 removes the throw-away caps and places fresh protective caps on the Temporal Artery Thermometer
These are the steps to follow (see infographic):
Step 1 – Scanner #1 picks up Temporal Artery Thermometer #1
Step 2 – Scanner #1 places a protective throw-away cap on the sensor of the Temporal Artery Thermometer
Step 3 – Scanner # 1 scans person #1 after wiping away any hair. Just a gentle swipe across the forehead is all that needs to be done to perform a perfect measurement
Step 4 – Scanner #1 releases the button to read the temperature of person #1
Step 5 – Scanner #1 gives thermometer #1 to scanner #2 and picks up thermometer #2
Step 6 – Using Temporal Artery Thermometer #2 scanner #1 scans person #2. Meanwhile scanner #2 removes the protective throw-away cap from Temporal Artery Thermometer #1 and replaces it with a fresh protective cap
Step 7 – Scanner # 1 releases the button on the Temporal Artery Thermometer #2 to read the temperature of person #2
Step 8 -Scanner #1 gives Temporal Artery Thermometer #2 to scanner #2 and picks up Temporal Artery Thermometer #1 to start scanning person #3. Scanner #2 removes the protective cap from Temporal Artery Thermometer #2 and replaces it with a fresh cap
Cautionary remark: timing is everything
Fever-range temperatures occur about half as common during mornings as during evenings. That is one of the conclusions researchers come to in a recent study called ‘Fever Are Rarest In The Morning: Could We Be Missing Infectious Disease Cases by Screening for Fever Then?’. In the study researchers have retrospectively investigated fever-range temperatures (≥ 100.4 F or ≥38,0 oC) during seasonal influenza outbreaks and the 2009 H1N1 (swine flu) pandemic. These same data sets have recently been used as preparatory models for the COVID-19 pandemic. The analyses included data from a nationally representative sample of records from adult visits to US emergency departments and data from a Boston based emergency department.
Additional screening might be necessary
Currently fever screening is usually recommended once daily at morning arrival. But this study suggests this might not be enough. The morning hours might even be “the worst time” for screening visitors and employees for fever, the researchers state in a discussion of their results. They suggest a new procedure might be necessary where people are being measured at both start and end of their shift or workday. During extended shifts we should look at taking temperature at least every 12 hours.
How does an adjusted temperature measurement procedure work?
The first measurement in the morning would make it possible to screen and detect cases before the shift or workday starts.
The second screening would help catch cases previously missed.
